Admitted to Hospital for Observation is it Covered?







If you’re admitted to a hospital for observation and not for treatment of a specific ailment, are expenses covered?







If you’re admitted to a hospital for observation and not for treatment of a specific ailment, are expenses covered?
All health insurance plans must covered the cost of a breast pump, either as a rental or a new one. Breastfeeding support, counseling, and equipment for the duration of breastfeeding are all covered.
If ObamaCare is repealed in full, then millions will lose coverage and both healthcare costs and federal spending on healthcare will go up.
Preventive services are covered under the ACA, but there are a few important things to understand about how preventive services work.
The ACA gives over 30 million Americans coverage options, lowers costs for the 1 in 2 with preexisting conditions, but increased costs for some who had insurance before.
An insurer will only pay up to an allowed amount each time you receive a covered service. There is no lifetime or annual limits to the amount they will spend doing that
TRICARE is subject to the elimination of copayments for authorized preventive services for certain TRICARE beneficiaries for non-grandfathered plans.
There are a number of insurers who offer transgender health coverage. The ACA helps transgender Americans due to its many patient protections.
Non-payment is the only way, aside fraud, to get your health plan dropped. Generally you have no less than 31 days to make a payment while your plan still pays claims.
If a spouse doesn’t have access to an employer plan and is turning 26 they can get a Marketplace plan based on household income.
Rules pertaining to electronic health records were established in the PPACA in sec. 3003.
Does Obamacare cover abortions and contraception?
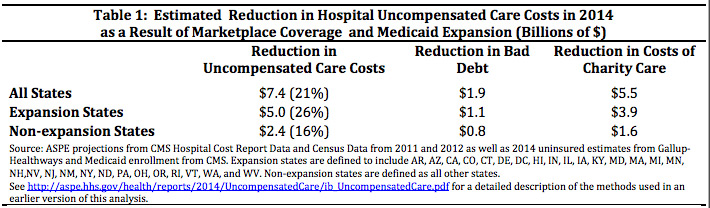
According to HHS the expansion of Medicaid and the increased coverage under the ACA has led to a reduction in unpaid medical bills saving taxpayers and hospitals billions. Highlights from the factsheets can be found below (for a list of citations see page 3 of this PDF). NOTE: This information is from a 2015 report. Logically… Read More
Children can stay on their parent’s plan until 26; when they turn 26, they qualify for special enrollment. Additionally, many employers offer dependent coverage for young adults. Below is a comprehensive guide to the Affordable Care Act’s provisions for young adults under 26, ensuring they maintain access to health insurance coverage. What the ACA Does… Read More
US citizens can enroll in ObamaCare’s Health Insurance Marketplace via Special Enrollment when retuning to the US after living abroad.
States can use funds from SEC. 10211. of the ACA to subsidize formula for new mothers. Formula can also be a medical expense, but is typically not a covered benefit.
No insurer can deny you for preexisting conditions, once you start the plan all treatment is covered. Treatment sought before your plan started isn’t covered, but ALL treatment that counts as a covered benefit is covered at the plans cost sharing amount.
Those who are incarcerated are exempt from the requirement to have health coverage, once a person leaves incarceration it triggers a special enrollment period to use the Marketplace.
All non-grandfathered plans sold after 2014, that count as comprehensive coverage, have to cover preexisting conditions without exclusions or look-back periods.
No one loses coverage, for any reason, other than non-payment or fraud. Coverage is guarantee issue, and the ratio of what someone can be charged based on age is 3 to 1.
In the case where a child needs immediate attention, but was dropped from their insurance plan, they should call the Marketplace and seek help at a hospital.
Yes. Since cancer screenings are a preventive service (one of ObamaCare’s Minimum Essential Benefits), all ObamaCare health insurance plans have to cover lung cancer screenings. In most cases, this service must be offered at no out-of-pocket costs.
When someone turns 26 they can apply for ObamaCare before their 26th birthday allowing the plan to start when they turn 26. Get the details below.
TRICARE and VA coverage are excluded from some ACA rules including the rule for staying on a parents plan until 26. You can learn more about what parts of the ACA TRICARE and VA coverage embrace and what rules are specific to those insurance types here: http://fas.org/sgp/crs/misc/R41198.pdf.
The rate review provision is overseen by the state, the Medical loss ratio is overseen by HHS.