ACOs (Accountable Care Organizations)







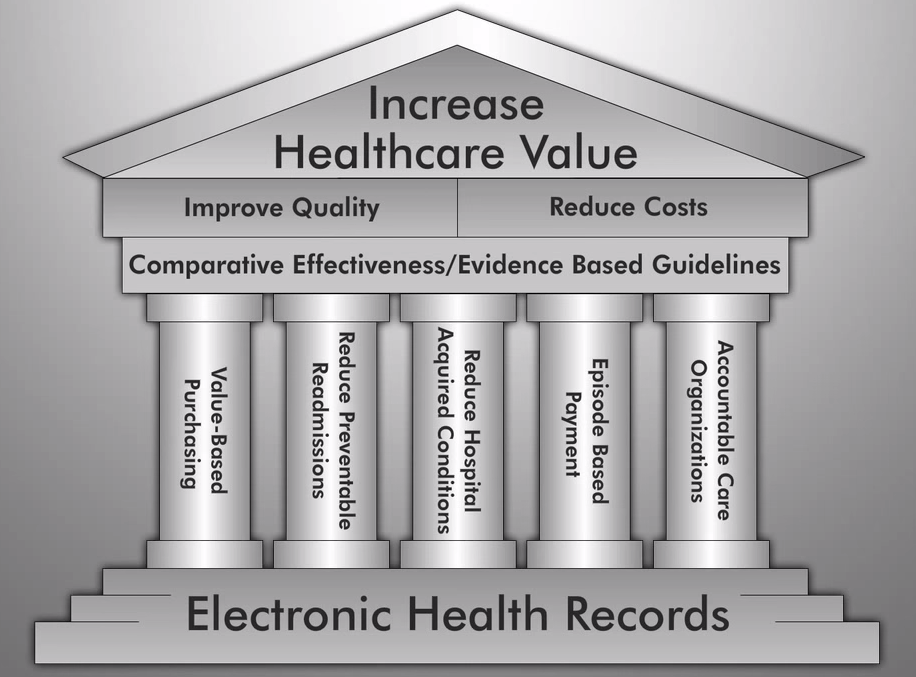
Account Care Organizations (ACOs) are groups of medical providers that accept payments based on quality under the Medicare Shared Savings Program (MSSP). This model is meant to be an alternative to the traditional fee-for-service (FSS) aimed at reigning in unnecessary treatments, coordinating care, promoting quality over quantity, and curbing Medicare spending.
The Affordable Care Act Accountable Care Organizations and the Medicare Shared Savings Program
ACOs were created by sec. 2706 of the Patient Protection and Affordable Care Act to take part in the Medicare Shared Savings Program created under sec. 3022. An ACO, which can include primary care physicians, specialists, hospitals or other providers, bears responsibility jointly for the cost and quality of care delivered to a subset of Original Medicare beneficiaries. If they hit the quality targets, any savings that result are then shared among the providers, on that same token if they miss targets they can end up owing money back to Medicare.
Initial reports show that overall the model is effective, but some of the initial “Pioneer ACOs” reported losses for one or more years. Despite this in 2013, ACOs were projected to save Medicare up to $940 million in the first four years. MSSP and ACOS are part of an overall focus on quality over quantity in order to reduce Medicare spending.
As of 2015 there were already 360 ACOs within the Medicare program serving about 5.3 million beneficiaries (about 12 to 13 percent of all people with Medicare). The number of ACOs has been growing by about 100 organizations each year.
The ACO Payment Model
ACOs get paid based on their patients’ medical outcomes rather than on how many tests and procedures they perform. Under the Pioneer model ACOs are paid at fee-for-service rates, but then can earn payments or have to pay-back money based on patient outcomes. There are a few different models for ACOs which you can read about in detail here.
The ACA Establishes ACOs, MSSP, and Other New Patient Care Models
ACOs and MSSP go hand-in-hand. You can find summaries of the sections below. PPACA Title II Part III also includes other pilot programs and innovations for new patient care models aimed at improving quality of care and keeping costs down. See a full summary of all PPACA provisions here.
Sec. 2706. Pediatric Accountable Care Organization demonstration project. Establishes a demonstration project that allows qualified pediatric providers to be recognized and receive payments as Accountable Care Organizations (ACO) under Medicaid. The pediatric ACO would be required to meet certain performance guidelines. Pediatric ACOs that met these guidelines and provided services at a lower cost would share in those savings.
Sec. 3022. Medicare shared savings program. Rewards Accountable Care Organizations (ACOs) that take responsibility for the costs and quality of care received by their patient panel over time. ACOs can include groups of health care providers (including physician groups, hospitals, nurse practitioners and physician assistants, and others). ACOs that meet quality-of-care targets and reduce the costs of their patients relative to a spending benchmark are rewarded with a share of the savings they achieve for the Medicare program.
ACO and MSSP Creation and Pilot Programs
The initial run of this from 2012 – 2013 was known as the Pioneer model, the first 32 ACOs created are known as Pioneer ACOs. Each ACO could pick from two tracks: track 1 is a sharing-only arrangement, while track 2 puts providers at risk for increased costs.
How Much are ACOs Saving Medicare?
32 organizations, considered ‘Pioneer ACOs’, began using the ACO model back in 2012. An independent evaluation report has shown that between 2012 and 2013 the ACO model saved about $300 per Medicare beneficiary for a total of $384 million ($279.7 million in 2012; $104.5 million in 2013).
While that number might not seem like that much, in practice if the model were expanded it could be just what is needed to bring the rising cost of Medicare spending down over time. Bringing Medicare spending down (if no other changes are made to other spending and revenue) would go a long way to decreasing the deficit.
See page ii of the CMS report on ACOs for more facts on how the Pioneer ACO model is working.
For more recent 2014 numbers see the latest August 2015 ACO report from CMS here.
Track 1 Versus Track 2
ACOs may participate in the Medicare Shared Savings Program (MSSP), also known as the Pioneer Model. The MSSP program contains two tracks: track 1 is a sharing-only arrangement, while track 2 puts providers at risk for increased costs. Under the current MSSP program, all ACOs—whether participating in track 1 or track 2—will have to assume risk by the second agreement period. The Pioneer Model is currently authorized through 2016 and offers an even greater transfer of risk than track 2 of MSSP. The expansion of the Pioneer Model would create an additional option for ACOs that would also require providers to accept risk.
What Isn’t Working with ACOs?
Not all of the 32 ACOs that began the pilot program continued it. While some of the ACOs saw substantial savings and overall the pioneers saw substantial savings some ACOs actually lost money in one or more years. The focus is on treating patients efficiently and thus providing better care with less costly services, but some ACOs ended up needing to provide more care than the lump-sum payment covered.
The Pioneer Model began on January 1, 2012. It featured 32 Pioneer ACOs choosing 3-year agreements, with optional 2-year extensions, under one of five financial tracks that offered varying sequential pathways to an elevated transfer of financial risk for the cost of Part A and B claims and reported quality-of-care measures for annually aligned FFS beneficiaries. Of those 32 ACOs, 23 remained in the Model through the conclusion of the second performance year (2013), and 19 continue to participate as of the first quarter of the fourth performance year (2015).Eight of the 13 no longer participating in the Pioneer Model have since transitioned into MSSP. – Read the full April 10, 2015 Report on ACOs from CMS