GOP Budget Includes $1.8 Trillion in HealthCare Cuts







A GOP budget resolution that just passed the House includes $1.8 trillion in healthcare cuts and $1.5 trillion in tax cuts over a ten year period.







A GOP budget resolution that just passed the House includes $1.8 trillion in healthcare cuts and $1.5 trillion in tax cuts over a ten year period.
The CBO says the Bipartisan Health Care Stabilization Act of 2017 would cut the deficit by $3.8 billion over ten years and would not substantially change uninsured rates.
Trump’s move to cut Cost-Sharing Reduction assistance will likely result in lower premiums for those who qualify for Premium Tax Credits on Bronze, Gold, and Platinum plans.
Just a reminder, Medicare Open enrollment 2018 is here. Enrollment goes from October 15th to December 7th each year. Coverage starts January 1st.
Although there is no fix passed, some and Congress and Trump have discussed a bipartisan fix for ObamaCare’s cost sharing subsidies.

The White House announced that the Trump administration will no longer reimburse insurers for ObamaCare’s cost-sharing reduction subsidies.
President Trump signed an executive order on Oct 12, 2017 to expand access to “association health plans,” to expand these across state lines, to expand short-term coverage, and to expand HRAs.
The House GOP’s proposed 2018 budget cuts healthcare and other social funding to offset new tax cuts (i.e. it does what all GOP legislation does.)

The Trump administration will expand exemptions to an ObamaCare rule requiring employers to provide plans that cover birth control.
Word is Trump plans to reject a “stopgap” plan in Iowa to control premiums and save their insurance market. However, no official decision has been made yet.
Below is a copy of the 2015 study published on HHS, “The Potential Fiscal Consequences of Not providing CSR Reimbursement.”

Congress failed to fund the Children’s Health Insurance (CHIP) for 9 million kids and 1,400 Community Health Centers by the Sept. 30 2017 deadline.
As of Sept. 29 2017 Congress has yet to fund CHIP (the Children’s Health Insurance Program that covers about 9 million kids). CHIP expires Sept. 30, 2017.
Trump indicated he would allow insurers to sell across state lines, this idea was in his campaign platform and can be done by executive order.

A bipartisan bill known as the CHRONIC Care Act passed the Senate Tuesday night. The bill aims to expand the Affordable Care Act and improve Medicare.

Graham-Cassidy Repeal and Replace Bill Won’t Be Voted On The Senate won’t vote on the Graham-Cassidy Bill to replace ObamaCare (the Affordable Care Act), as the bill lacked the votes to pass. This was decided after Majority Leader Mitch McConnell met with lawmakers to see where Senators stood on the proposal. Previously Sen. Susan Collins, a Republican… Read More

At a webinar for assisters, HHS announced that HealthCare.Gov would shut down between 12am – 12pm EST on Sunday mornings during open enrollment.
The Cassidy-Graham bill has been estimated by studies to result in 32 million uninsured by 2027 and beyond and higher costs for many sick, poor, and seniors.

Rand Paul opposes the Graham-Cassidy bill to repeal and replace ObamaCare, not because it cuts too much, but because it doesn’t cut enough.

We explain the gist of the Graham-Cassidy Obamacare repeal bill. In short, it looks a lot like the last repeal attempt, the Better Care Reconciliation Act.
Bernie’s Medicare-for-all bill ignores funding, but not as an oversight. The bill itself purposefully leaves funding mechanisms open to debate.

Deferred Action for Childhood Arrivals (DACA) recipients are not eligible for ObamaCare, don’t have to comply with the mandates, can’t use the marketplace, and can’t get cost assistance.

The Trump administration cut ObamaCare’s advertising and outreach budget sharply this year. Ad funding was reduced from $100 million to $10 million.
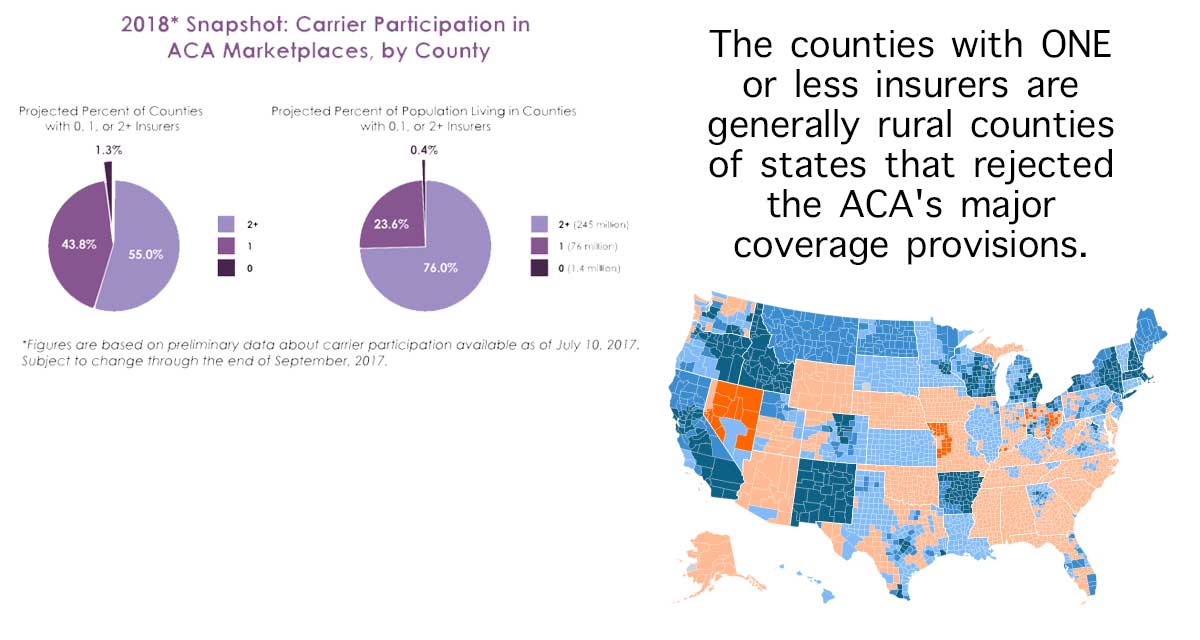
Although only a few states have a number of ObamaCare insurers offering plans, some have only one or two. We explain what this means.
We explain the August 15, 2017 CBO and JCT report on the effects of ending cost-sharing reduction payments to insurers.